What enables successful dental hygiene systems integration: An RNA180 case study
Background
Successful system integration in dental practices rarely hinges on the software itself. Outcomes are shaped by the conditions into which a system is introduced: leadership alignment, clinical trust, workflow readiness, and the presence of support rather than enforcement. When those elements exist, integration becomes less about change management and more about stabilising how care is planned and delivered. This case study examines what successful system integration looks like in practice, using RNA180 dental hygiene management software as a reference example.
This particular dental clinic was recently acquired by a client who already had several other clinics ultilising RNA180. It is a multi provider dental practice with a strong dental hygiene team and leadership committed to clinical standards, operational clarity, and long-term practice value. However, like many practices, they faced a familiar challenge: their dental hygienists were clinically capable and engaged, yet dental hygiene performance showed variability across providers. Due-but-missed opportunities remained high, appointment lengths were inconsistent, and production per hour did not reflect the level of care being delivered.
Leadership understood that the issue was not effort or intent but clinical systems and workflows. Treatment planning relied heavily on memory, habit, and time pressure. Standardisation was difficult to achieve without increasing administrative burden, and coaching opportunities were hard to pinpoint without reliable data.
Recognising these challenges as ones they had faced in the past with their other locations, this office implemented RNA180 to introduce a consistent, clinician aligned planning system that supported dental hygienists in real time while providing leadership with visibility into dental hygiene performance.
Implementation and Early Adoption
RNA180 was integrated into the practice and training was completed across the dental hygiene team. Within the first week post implementation, adoption exceeded expectations. Four of six dental hygienists were planning 100% of the time and pre planning most appointments. A fifth provider reached 66% usage after a slower start. One provider initially did not engage, highlighting a common reality in any change initiative.
Despite partial adoption, early indicators were immediately positive.
Within the first week, dental hygiene performance metrics began to shift. Due but missed treatment dropped across multiple categories, and hygiene production per hour increased significantly. This early lift occurred before any formal coaching or optimisation, underscoring the impact of simply planning consistently with a system that supports consistent clinical practise.
Quantifiable Outcomes
Over the first 90 days, and through to support of leadership, this practice saw sustained, measurable improvements across dental hygiene performance metrics. Let’s have a closer look at those outcomes.
Dental Hygiene Production Per Hour
Baseline data from the previous quarter showed an all-in hygiene hourly average of approximately 224 (June to August) dollars per hour (this number includes all exams and rads performed in the chair). By the first month post implementation, this had increased to approximately 301 dollars per hour and remained stable through month two and three. This represents an average sustained increase of 77 dollars per hour without extending appointment times or increasing patient volume and an increase of over 100k of additional dental hygiene revenue, over the quarter. Simply outstanding.
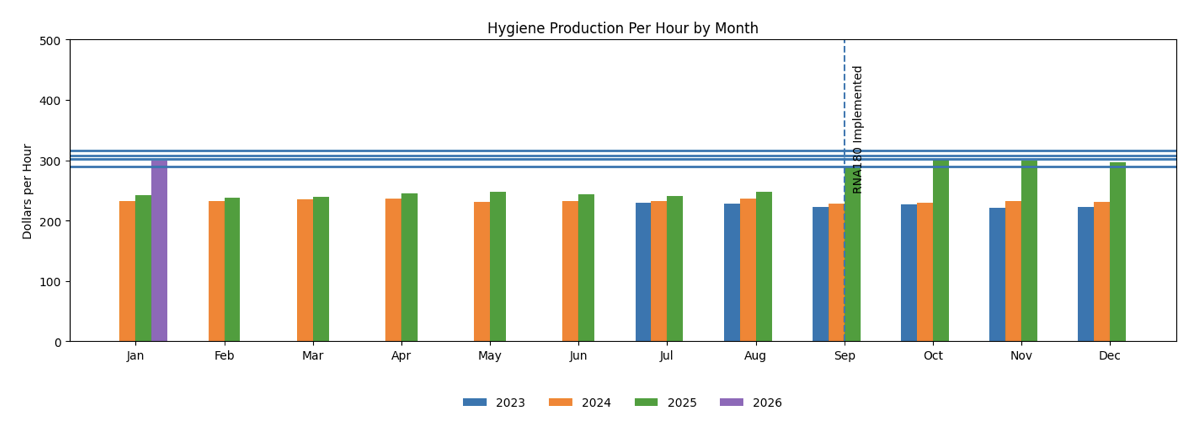
Figure 1: RNA180 Implementation Sept 2025
Raw hygiene production (dental hygiene services only) increased by approximately 34 dollars per hour, rising from 170 dollars to 204 dollars. These figures reflect true chairside time, not inflated scheduling assumptions.
Individual provider gains were equally notable. One dental hygienist achieved an 83 dollar per hour increase. Others consistently realised gains between 55 and 70 dollars per hour. Importantly, these improvements were driven by more accurate planning and billing rather than rushing care or overbooking providers.
Due-But-Missed Treatment
At baseline, due but missed treatment rates were high. Pan sat at over 93% missed. Bitewing radiographs approached 46%. Comprehensive oral exams exceeded 40%. Probing was missed in over 50% of cases.
Within the first month, these figures dropped dramatically. Probing fell to 36%. Bitewings dropped to 28%. Comprehensive exams reduced to 29% and pans to 38%. By month two, most categories remained stable or continued to improve, demonstrating that the behaviour change was sustained rather than short lived and the driving change behind the improvements in standard of care.
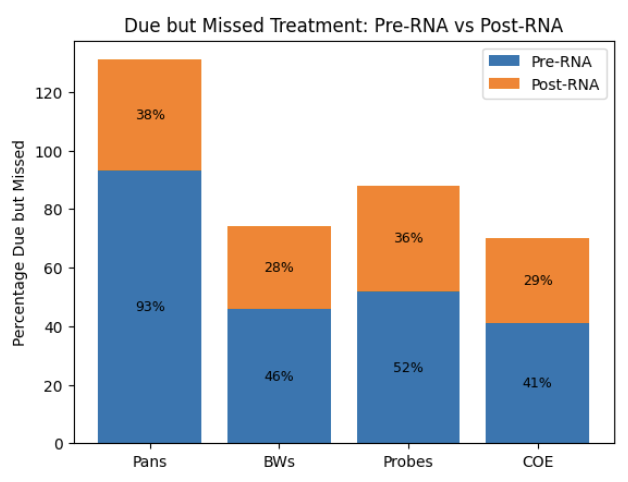
Figure 2: Due-but-Missed Improvements
These improvements were achieved through consistent preplanning, visible clinical prompts, and the ability for dental hygienists to customise care intervals appropriately, within each patient profile.
Clinical Consistency and Behaviour Change
Beyond revenue metrics, RNA180 surfaced important insights into clinical behaviour. The data revealed where dental hygienists were undervaluing their time, particularly around scaling units. Several providers routinely reduced billed scaling despite performing the work. Others used sterilisation or other codes as buffers when appointment lengths felt tight.
With visibility came opportunity. Leadership could now coach based on facts rather than assumptions. In several cases, dental hygienists corrected these patterns within weeks once they saw the data and understood the impact on both patient care and practice performance.
The system also highlighted scheduling inefficiencies. Fifteen-minute scheduling increments were shown to be too coarse for effective optimisation. Many appointments defaulted to 60 minutes when 50 minutes would have been more appropriate, creating unnecessary time pressure and adjustment downstream. Conversely, many more appointments were shown to be simply too short for the due treatment, highlighting the importance of building appointments to actual need vs defaulted 60 minutes.
These insights allowed leadership to address root causes rather than symptoms.
Team Engagement and Culture
Importantly, adoption improved over time. By month two, five of six dental hygienists were planning at 95% or higher, with an average usage rate of 98%. Even initially hesitant providers began engaging with the system, often with peer support or light coaching.
The tool did not replace clinical judgement. It supported it. Dental hygienists continued to individualise care while benefiting from consistent prompts and reduced cognitive load. Notes improved in quality. Interval management became more accurate. Planning became proactive rather than reactive.
This shift reduced friction, improved confidence, and allowed dental hygienists to focus on care rather than mental arithmetic and administrative burdens.
Leadership Value and Practice Impact
For leadership, RNA180 delivered something critical. Predictability.
Hygiene performance became measurable, explainable, and coachable. Variability between providers narrowed. Revenue became more defensible because it reflected care delivered rather than chance or memory. Clinical standards were easier to uphold without micromanagement.
From a practice value perspective, this matters. Consistent hygiene performance supports valuation, reduces dependency on individual providers, and demonstrates operational maturity.
Key Takeaways
This practice’s experience illustrates several important truths.
- meaningful performance improvement does not require more patients or longer days. It requires better systems.
- dental hygienists respond positively to tools that respect their clinical autonomy and patient care while reducing administrative friction.
- data driven coaching strengthens culture rather than undermines it when positioned as support rather than surveillance.
Finally, hygiene performance is not just a clinical issue. It is a business driver that directly influences practice stability and value.
Within 90 days, this office like many of our clients transformed their dental hygiene team into a more consistent, confident, and predictable engine of care and revenue using RNA180. Ultimately, successful system integration is enabled by leadership that creates an environment which allows the system to do what it is designed to do.
Quick Links
© 2025 by RNA180- All Rights Reserved
Managing Teams at Scale
Leadership, systems & care for growing dental practices.
Watch the panel on demand.